Varicose Veins
Varicose veins are enlarged veins that can be blue, red, or flesh-colored. They are often raised above the skin on legs and look like twisted, bulging cords because of a defect with the leaflet valves inside the vein.
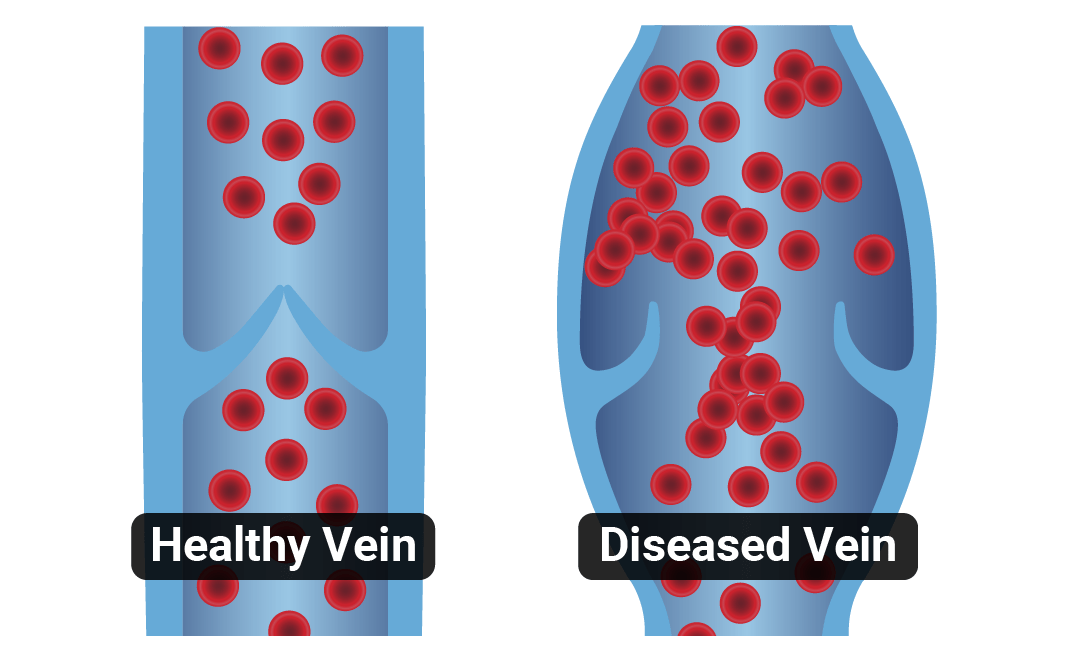
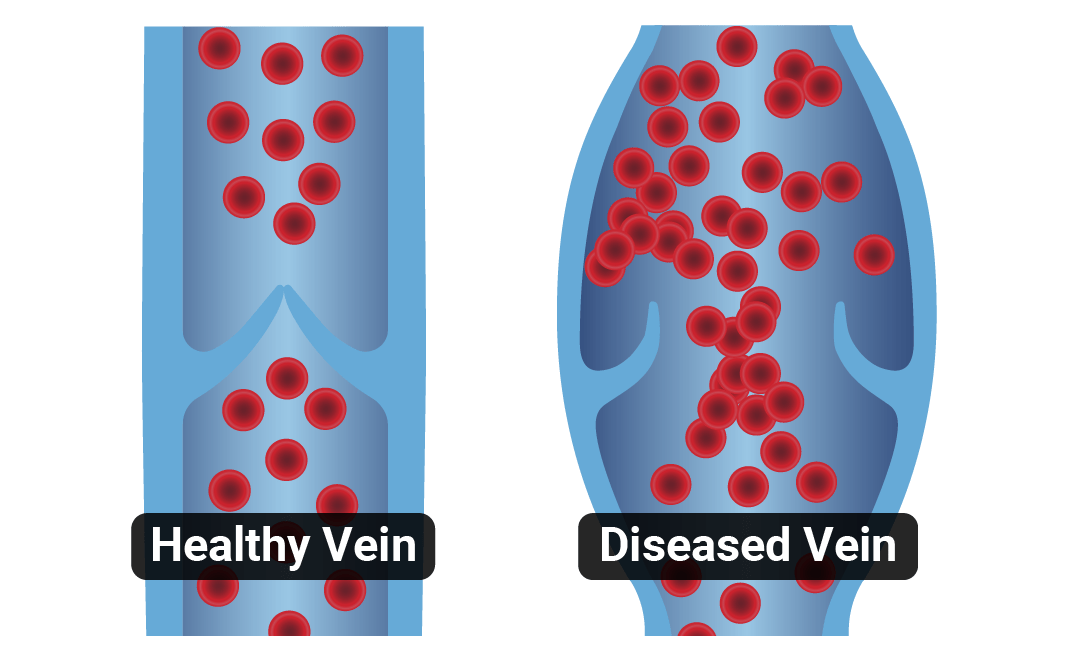
Normally, blood in the veins travels back to the heart in one direction (towards the heart) supported with the pump action of the calf muscles and one-way valves. These valves, when working normally, prevent blood from flowing backward. But sometimes the leaflets of the valves fail to meet properly, allowing blood to flow backward and cause the vein to expand.
They can also be associated with pain, aches, heaviness, restless legs, or burning and itching of the skin.
What Is Chronic Venous Insufficiency?
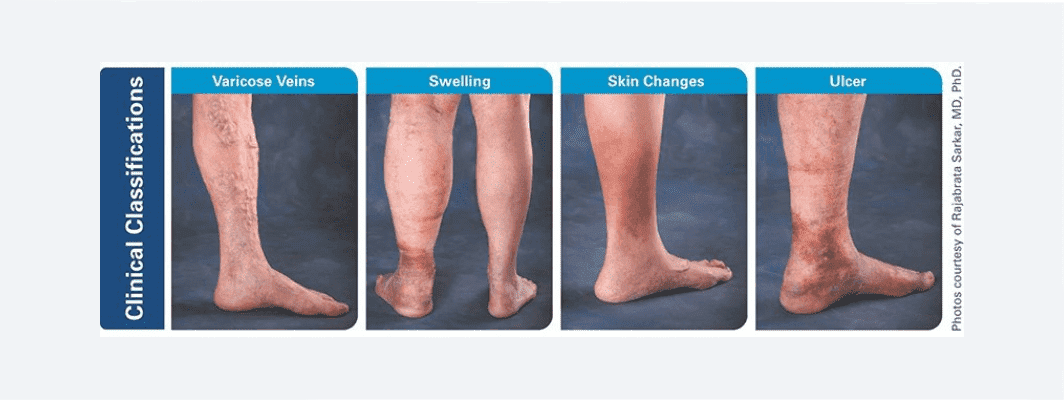
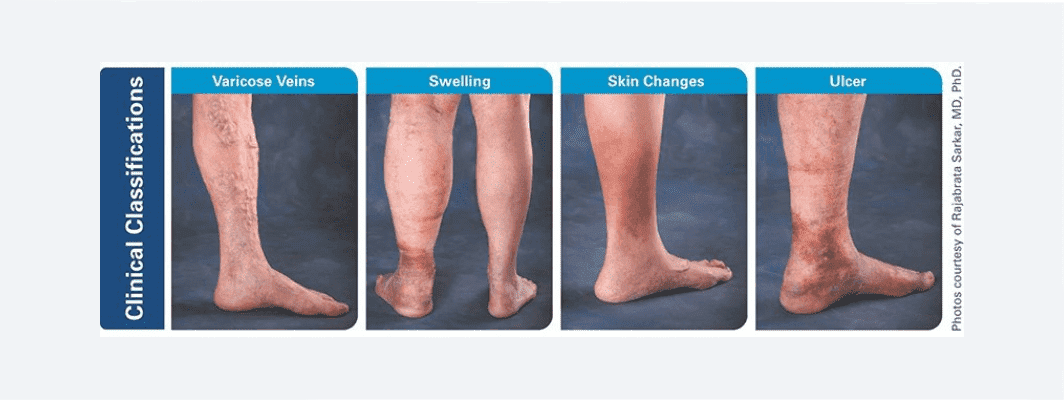
Chronic Venous Insufficiency (CVI) is a progressive medical condition that may worsen over time. As varicose veins progress to become CVI, other painful symptoms like leg swelling, skin damage, and ulcers may occur. There are a number of factors that contribute to varicose veins and CVI, including pregnancy and heredity.
Symptoms of Varicose Veins
- Veins that are dark purple or blue in color
- Veins that appear twisted and bulging; they are often like cords on your legs
Varicose veins are many times thought of as only a cosmetic problem. However, serious medical issues can arise if left untreated. Issues include:
- Heavy legs
- Itching and burning
- Lower leg swelling and pain (more pronounced at the end of the day)
- Night leg cramps
- Changes in skin color
- Leg ulcers
- Blood clotting
Often times, these symptoms are misdiagnosed or attributed to the natural process of aging. Varicose veins are present in 25% to 33% of female adults and 10% to 20% of male adults. In the US, chronic venous insufficiency (CVI) affects more than 30 million adults.
Causes of Varicose Veins
Varicose veins appear most commonly on the legs but can occur elsewhere. Causes of varicose veins include:
- Pregnancy
- Obesity
- Menopause
- Aging
- Leg injuries
- Prolonged standing or sitting
- Heredity
When Should You See A Doctor?
Elevating your legs, wearing compression stockings, and exercise can help ease the pain of varicose veins and prevent them from getting worse. But if you’re concerned about the way they look or are experiencing regular discomfort, there a number of treatment options that a doctor can perform.
Varicose Veins Treatments
Not every condition related to venous insufficiency requires treatment. You and your doctor should discuss your specific situation and the options that are best for you. Varicose vein removal treatments range from conservative, lifestyle-based approaches to more advanced outpatient treatment methods.
Superficial venous reflux disease treatment aims to reduce or stop the backward flow of blood. Superficial vein removal is a great way to treating the diseased vein, improving the overall blood flow and helping relieve symptoms. For some patients, compression stockings alone may improve blood flow. For other patients, closing or removing the diseased vein may be necessary to improve blood flow. Closing or removing the diseased vein directs blood to nearby healthy veins. Your doctor can help you decide which treatment option is best for you. Contact one of our doctors if you require varicose vein treatment in east Tennessee.
ClosureFAST™ Targeted Endovenous Therapy
The ClosureFast™ procedure is a minimally invasive segmental ablation treatment that utilizes radiofrequency (RF) energy to provide an even and uniform heat to contract the collagen in the vein walls, causing them to collapse and seal. Once the diseased vein is closed, blood will re-route itself to other healthy veins.
The ClosureFast™ procedure allows for a quick, comfortable recovery and a return to everyday activities for the average patient while also improving the appearance of varicose veins. The ClosureFast™ procedure has been proven in clinical studies to have excellent long-term effectiveness, with less pain and bruising than endovenous laser.
VenaSeal™ Closure System
The VenaSeal™ closure system is the first and only treatment approved for use in the US that uses an advanced medical adhesive to safely and effectively close the diseased vein segment. This improves blood flow by sealing or closing the diseased vein.
Unlike other heat-based treatments, the VenaSeal™ closure system does not require multiple injections of a dilute local anesthetic (tumescent anesthesia), enabling patients a more comfortable treatment therapy and allowing them to rapidly return to normal activities following the procedure. The VenaSeal™ closure system also eliminates the risk of burning or nerve injury associated with thermal based procedures and may not require the use of compression stockings post procedure.
The VenaSeal system has proven to have similar clinical results as the standard of care thermal treatment options.
Non-thermal, Non-tumescent Therapy
Varicose veins are a common condition and their management has undergone a number of changes over the years. Recently, new varicose vein treatment options have become available here in the U.S. These new treatment options do not require a heat source (non-thermal) to close the vein and, therefore, eliminates the need for the physician to use a tumescent (numbing agent). As non-thermal technology for saphenous vein ablation develops, patient experience should continue to improve. Because this therapy does not require numbing agents, the need for needle sticks is reduced.
Microambulatory Phlebectomy
Microambulatory Phlebectomy is an ancillary procedure that is typically reserved for removing remaining varicose veins that did not disappear after the treatment of refluxing superficial veins. On average, varicose veins will significantly reduce or disappear about 6 months after a refluxing vein is treated. The majority of patients do not need future phlebotomies.
It is a simple in-office procedure that involves minor surgical removal of any remaining bulging veins. The physician will map out the vein and numb the area using a local anesthetic. Small incisions are made along the length of the vein. With each small incision, a segment of the vein is removed using a specialized instrument similar to a crochet hook. Once the vein is removed, the incisions are closed with a steri-strip. The incisions heal in about a week and typically do not require sutures.
Potential Risks of Varicose Vein Treatments
The treatment for varicose veins is minimally invasive and catheter-based. As such, it may involve the following risks. Your doctor can help you understand these risks.
- Allergic reaction
- Arteriovenous fistula (i.e., an abnormal connection between an artery and a vein)
- Bleeding from the access site
- Deep vein thrombosis (i.e., blood clot in the deep vein system)
- Edema (i.e., swelling) in the treated leg
- Hematoma (i.e., the collection of blood outside of a vessel)
- Hyperpigmentation (i.e., darkening of the skin)
- Infection at the access site
- Non-specific mild inflammation of the cutaneous and subcutaneous tissue
- Pain/Achy Leg(s)
- Paresthesia (i.e., a feeling of tingling, pricking, numbness or burning)
- Phlebitis (i.e., inflammation of a vein)
- Pulmonary embolism (i.e., blockage of an artery in the lungs)
- Urticaria (i.e., hives) or ulceration may occur at the site of injection
- Vascular rupture and perforation
- Visible scarring
Varicose Veins
Varicose veins are enlarged veins that can be blue, red, or flesh-colored. They are often raised above the skin on legs and look like twisted, bulging cords because of a defect with the leaflet valves inside the vein.
Normally, blood in the veins travels back to the heart in one direction (towards the heart) supported with the pump action of the calf muscles and one-way valves. These valves, when working normally, prevent blood from flowing backward. But sometimes the leaflets of the valves fail to meet properly, allowing blood to flow backward and cause the vein to expand.
They can also be associated with pain, aches, heaviness, restless legs, or burning and itching of the skin.
What Is Chronic Venous Insufficiency?
Chronic Venous Insufficiency (CVI) is a progressive medical condition that may worsen over time. As varicose veins progress to become CVI, other painful symptoms like leg swelling, skin damage, and ulcers may occur. There are a number of factors that contribute to varicose veins and CVI, including pregnancy and heredity.
Symptoms of Varicose Veins
- Veins that are dark purple or blue in color
- Veins that appear twisted and bulging; they are often like cords on your legs
Varicose veins are many times thought of as only a cosmetic problem. However, serious medical issues can arise if left untreated. Issues include:
- Heavy legs
- Itching and burning
- Lower leg swelling and pain (more pronounced at the end of the day)
- Night leg cramps
- Changes in skin color
- Leg ulcers
- Blood clotting
Often times, these symptoms are misdiagnosed or attributed to the natural process of aging. Varicose veins are present in 25% to 33% of female adults and 10% to 20% of male adults. In the US, chronic venous insufficiency (CVI) affects more than 30 million adults.
Causes of Varicose Veins
Varicose veins appear most commonly on the legs but can occur elsewhere. Causes of varicose veins include:
- Pregnancy
- Obesity
- Menopause
- Aging
- Leg injuries
- Prolonged standing or sitting
- Heredity
When Should You See A Doctor?
Elevating your legs, wearing compression stockings, and exercise can help ease the pain of varicose veins and prevent them from getting worse. But if you’re concerned about the way they look or are experiencing regular discomfort, there a number of treatment options that a doctor can perform.
Varicose Veins Treatments
Not every condition related to venous insufficiency requires treatment. You and your doctor should discuss your specific situation and the options that are best for you. Varicose vein removal treatments range from conservative, lifestyle-based approaches to more advanced outpatient treatment methods.
Superficial venous reflux disease treatment aims to reduce or stop the backward flow of blood. Superficial vein removal is a great way to treating the diseased vein, improving the overall blood flow and helping relieve symptoms. For some patients, compression stockings alone may improve blood flow. For other patients, closing or removing the diseased vein may be necessary to improve blood flow. Closing or removing the diseased vein directs blood to nearby healthy veins. Your doctor can help you decide which treatment option is best for you. Contact one of our doctors if you require varicose vein treatment in east Tennessee.
ClosureFAST™ Targeted Endovenous Therapy
The ClosureFast™ procedure is a minimally invasive segmental ablation treatment that utilizes radiofrequency (RF) energy to provide an even and uniform heat to contract the collagen in the vein walls, causing them to collapse and seal. Once the diseased vein is closed, blood will re-route itself to other healthy veins.
The ClosureFast™ procedure allows for a quick, comfortable recovery and a return to everyday activities for the average patient while also improving the appearance of varicose veins. The ClosureFast™ procedure has been proven in clinical studies to have excellent long-term effectiveness, with less pain and bruising than endovenous laser.
VenaSeal™ Closure System
The VenaSeal™ closure system is the first and only treatment approved for use in the US that uses an advanced medical adhesive to safely and effectively close the diseased vein segment. This improves blood flow by sealing or closing the diseased vein.
Unlike other heat-based treatments, the VenaSeal™ closure system does not require multiple injections of a dilute local anesthetic (tumescent anesthesia), enabling patients a more comfortable treatment therapy and allowing them to rapidly return to normal activities following the procedure. The VenaSeal™ closure system also eliminates the risk of burning or nerve injury associated with thermal based procedures and may not require the use of compression stockings post procedure.
The VenaSeal system has proven to have similar clinical results as the standard of care thermal treatment options.
Non-thermal, Non-tumescent Therapy
Varicose veins are a common condition and their management has undergone a number of changes over the years. Recently, new varicose vein treatment options have become available here in the U.S. These new treatment options do not require a heat source (non-thermal) to close the vein and, therefore, eliminates the need for the physician to use a tumescent (numbing agent). As non-thermal technology for saphenous vein ablation develops, patient experience should continue to improve. Because this therapy does not require numbing agents, the need for needle sticks is reduced.
Microambulatory Phlebectomy
Microambulatory Phlebectomy is an ancillary procedure that is typically reserved for removing remaining varicose veins that did not disappear after the treatment of refluxing superficial veins. On average, varicose veins will significantly reduce or disappear about 6 months after a refluxing vein is treated. The majority of patients do not need future phlebotomies.
It is a simple in-office procedure that involves minor surgical removal of any remaining bulging veins. The physician will map out the vein and numb the area using a local anesthetic. Small incisions are made along the length of the vein. With each small incision, a segment of the vein is removed using a specialized instrument similar to a crochet hook. Once the vein is removed, the incisions are closed with a steri-strip. The incisions heal in about a week and typically do not require sutures.
Potential Risks of Varicose Vein Treatments
The treatment for varicose veins is minimally invasive and catheter-based. As such, it may involve the following risks. Your doctor can help you understand these risks.
- Allergic reaction
- Arteriovenous fistula (i.e., an abnormal connection between an artery and a vein)
- Bleeding from the access site
- Deep vein thrombosis (i.e., blood clot in the deep vein system)
- Edema (i.e., swelling) in the treated leg
- Hematoma (i.e., the collection of blood outside of a vessel)
- Hyperpigmentation (i.e., darkening of the skin)
- Infection at the access site
- Non-specific mild inflammation of the cutaneous and subcutaneous tissue
- Pain/Achy Leg(s)
- Paresthesia (i.e., a feeling of tingling, pricking, numbness or burning)
- Phlebitis (i.e., inflammation of a vein)
- Pulmonary embolism (i.e., blockage of an artery in the lungs)
- Urticaria (i.e., hives) or ulceration may occur at the site of injection
- Vascular rupture and perforation
- Visible scarring